Adrenoleukodystrophy: Bone Marrow Transplant Therapy
Bone marrow transplants have been used with the intention to treat storage diseases such as adrenoleukodystrophy The experiments that have been conducted has been shown to increase the life expectancy of patients that received the transplant compared to patients that did not.
Bone marrow transplantation works by the engraftment from normal donors providing cells that express a normal ratio of oxidation of C224:0 compared to C16:0. This graft has been shown to persist for as long as 8 years. The rationale for BMT in X-ALD has relied on the hypothesis that functional bone-marrow cells from the donor could cross the blood-brain-barrier in the recipient and exert favorable effects on the mechanisms leading to demyelination. Subsequently, short-term benefits of BMT in childhood cerebral X-ALD were reported.
This graph demonstrates the post-BMT effects in four patients with adrenoleukodystrophy. The shaded regions correspond to abnormal C24/16 ratio. In each graph it shows that after a bone marrow transplant the recipient show a normal C24/16 ratio.
Other neuropsychological evaluations have shown that patients destine to develop the severe form of childhood onset of cerebral adrenoleukodystrophy who receive a bone marrow transplant show evidence of stability and/or improvement, especially in verbal memory.
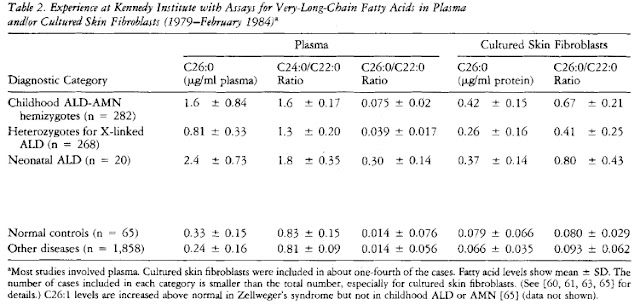
MRI observations have also indicated an abatement of the degenerative processes in the brain compared to transplanted patients. In the experiment done by Shapiro et. al, 2000, 12 patients with childhood onset of adrenoleukodystrophy were followed for 5-10 years after a bone marrow transplant. MRI showed complete reversal of abnormalities in two patients and improvement in one. One showed no change and all 8 patients who showed an initial period of continued demyelination stabilized and remained unchanged thereafter. Motor function remained normal or improved after BMT in 10 patients. Verbal intelligence remained with in the normal range for 11 patients. Plasma VLCFA concentrations decreased by 55% and remained slightly above the upper limit of normal.
This study of twelve transplanted and grafted cerebral X- ALD patients confirms the long-term beneficial effect of BMT when done early in the disease course.
Krivit et. al (1995) performed an experiment with 5 sets of brother in the same family who both have a likelihood of developing childhood adrenoleukodystrophy. The younger brothers of each pair were given the bone marrow transplant. In each, the non-transplanted patient has dies and the transplanted patient remained alive.
Presymptomatic patients are now being treated via two methods:
1) Bone marrow transplantation
2) Dietary manipulation as well as GTE:GTO supplementation to provide normalization of plasma VLCFA. There is hope that presymptomatic individuals who are on the diet may inhibit the onset of neurological deterioration
Things to consider before a bone marrow transplant:
- Correction of increased VLCFA is recommended before transplantation. Cell membrane are abnormal when VLCFA are elevated, red blood cells are an example. In high plasma VLCFA erythrocytes have higher mechanical fragility. When VLCFA in the plasma is within the normal reference range this fragility disappears.
- When C26:0 is below 0.4 ug/ml there has been minimal difficulty during the transplantation. If these levels are increased however difficulties have occurred. To solve this problem artificial lipid emulsions should be excluded.
- Platelet number ad function is also disrupted during dietary restriction and use of Lorenzo’s oil. The diet should be discontinued when transplantation is begun as well as addition of mandatory platelet transfusion.
- Severe and obvious neurological disabilities have been showed to lead to increased deterioration with bone marrow transplants. Eligibility should be carefully evaluated
- Graft rejection has also caused disadvantages to this procedure. The removal of T cells by elutriation will increase the availability of donors for those without HLA sibling or unrelated phenotypic identical ones.
After the transplantation it has been prescribed that no dietary restrictions need to be taken. No correlation of IQ with VLCFA subsequent to bone marrow transplantation has been found. Post transplantation data has indicated that all of the patients have elevated levels of VLCA despite full engraftment as measured by donor DNA and normal levels of oxidation activity of white cells.
Future goals for this therapy is to increase the use of elutriation of non-genotypic marrow and of cord-blood hematopoietic stem may vastly increase sources for donor cells, which will allow greater freedom from therapeutic decision making.
References
Krivit, W., Lockmam, A., Watkins, P., Hirsch, J. & Shapiro O. 1995. The future for
treatment by bone marrow transplantation for adrenoleukodystrophy, metachromatic leukodystrophy, globoid cell leukodystrophy and Hurler syndrome. The Jornal of Inherited Metabolic Diseases, 18; 398-412.
Shapiro, E., Krivit, W., Lockman, L., Lambaque, I., Peters, C., Cowan, M., Harris, R., Blanche, S., Bordigoni, S., Loes, D., Ziegler, R., Crittenden, M., Ris, B., Cox, C., Moser, H., Fischer, A. & Aubourg, P. 2000. Long-term effect of bone-marrow transplantation for childhood-onset cerebral X-linked adrenoleukodystrophy. The Lancet, 356; 713 - 719.
Alisha M.